Key Differences Between SI Joint Pain and Sciatica (Symptoms, Pain, Treatments & More)
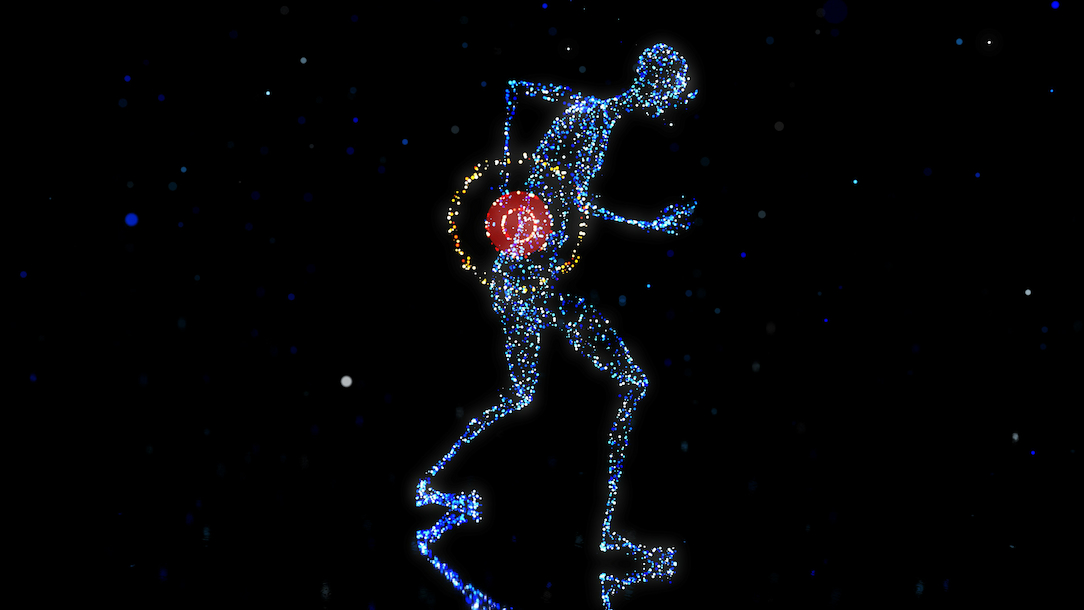
When you feel low back or buttock pain that seems to travel down your leg, it’s easy to jump to conclusions. You might think you have sciatica, but sometimes it’s actually your sacroiliac (SI) joint acting up.
In this article, we explain the differences between sciatica and SI joint pain so that you can better understand what might be going on with your body.
We break down the origins, sensations, triggers, and treatment paths so you can see the true contrast between these two common pain sources.
Shared Symptoms, but Very Different Sources
A big reason people get confused is that both conditions often overlap in the way they feel. You might experience pain while sitting, standing, walking, or after long periods of inactivity
There can be discomfort in your lower back, hips, buttocks, or groin that seems to rip or radiate down the leg.
That similarity can mask the real difference between sciatica vs. SI joint pain, but knowing how to discern them changes everything.
Where The Pain Is Coming From
On one side, SI joint pain arises from the joint connecting your sacrum (base of spine) to the ilium (pelvis).
If that joint is inflamed, misaligned, or has dysfunctional motion (too much or too little), it can generate pain in the pelvic region and lower back.
On the other side, sciatica refers to irritation or compression of the sciatic nerve or nerve roots in the lower lumbar or sacral spine.
That nerve runs from the lower back down through the buttocks, thighs, calves, and sometimes into the feet.
So while SI joint dysfunction is a mechanical or joint-structure problem, sciatica is fundamentally a nerve issue(or at least involves nerve pathways).
How The Pain Feels and Travels
Because of the different origins, the sensations often differ. With SI joint pain, you might feel a deep, dull ache or stiffness localized near the pelvis or lower back, often on one side.

Movements like standing up from sitting, walking, or shifting weight can aggravate it. It tends not to follow a strict nerve path and often doesn’t extend far below the knee.
With sciatica, on the other hand, the pain tends to be sharper, burning, or even electric shock-like.
It follows the path of the sciatic nerve, so the pain (or numbness, tingling, and weakness) can travel down the back of the thigh, calf, and into the foot. It often crosses known dermatomes and can produce true neurological signs (weakness or reflex changes).
Because both can cause discomfort down the leg, many people wonder about the difference between SI joint pain and sciatica, especially when the pain seems very similar.
Clues You Can Notice in Day-to-Day Life
To figure out what might be going on, you can pay attention to how your symptoms behave:
1. Triggering factors: If standing up from sitting or twisting your pelvis causes sharp pain in the pelvic region or buttock, that may hint at SI joint involvement. Prolonged sitting or weight shifting often worsens it.
2. Radiation pattern: If the pain goes below the knee or into the foot with numbness or weakness, it is more likely a nerve issue/sciatica. If it stays above the knee or is less structured, it could be the SI joint.
3. Neurological signs: True weakness, reflex changes, or sensory loss suggest nerve root involvement (sciatica). Joint problems seldom produce true neurological deficits.
4. Provocative tests: Certain physical tests (provocative maneuvers on the SI joint) may reproduce pain in that joint area. For nerve compression, tests like the straight leg raise or other nerve tension tests often reproduce leg symptoms.
By paying attention to those clues, you can better differentiate sciatica and SI joint pain, which is the first step to getting treatment and feeling better.
How Treatments Diverge
Because the cause differs, the treatment path also diverges.
Managing SI joint pain usually involves manual therapy to restore movement and alignment of the joint, strengthening of core and pelvic stabilizers, gentle exercises, and corrective posture. Sometimes, joint injections or supportive belts are used as additional tools if needed.
Treating sciatica focuses on relieving nerve compression: stretching, decompression, nerve gliding, addressing disc or spinal issues, specific manual therapy for sciatica, and sometimes more invasive interventions if conservative care doesn’t help.

Mistreating one as the other can delay recovery, so getting the right diagnosis is crucial. Recognizing the difference between sciatica and SI joint pain helps guide therapists and patients to the most effective interventions earlier.
Long-Term Relief and Preventing Recurrence
Once you know the root cause, you can adopt habits that reduce future flare-ups:
For SI joint issues, focus on strengthening hip & glute muscles, stabilizing your pelvis, maintaining balanced leg length, and avoiding asymmetrical loads or twisting.
For sciatica, incorporate core stability, lumbar posture, stretching of tight hamstrings or glutes, and movement strategies that reduce nerve irritation (avoid prolonged flexion or positions that pinch nerve roots).
In both cases, maintaining an active lifestyle, improving posture, and using proper ergonomics helps reduce the recurrence of low back or leg pain.
Clear Insight Leads to Better Recovery
You now see how two seemingly similar pain experiences can have totally different origins.
While they may share overlapping symptoms, understanding the difference between SI joint pain and sciatica is key to finding the right diagnosis, treatment, and long-term relief.
Once you know whether the problem stems from joint dysfunction or nerve compression, you can follow a tailored plan and speed up your recovery.
Ready to Reclaim Your Mobility?
If you’re dealing with persistent lower back or leg pain and want expert guidance, our team at Expert Manual Therapy offers personalized manual therapy,therapeutic exercises, and physical therapy tailored to your specific condition.
Reach out today to schedule an evaluation and start your journey toward pain-free movement.